Gastroscopy (Upper Endoscopy)
A gastroscopy is a key procedure to investigate upper gastrointestinal symptoms and detect digestive conditions, including cancer, at an early and more treatable stage. It helps identify the cause of symptoms such as persistent stomach pain, heartburn, bloating and difficulty swallowing.
Richmond Gastroenterology Centre
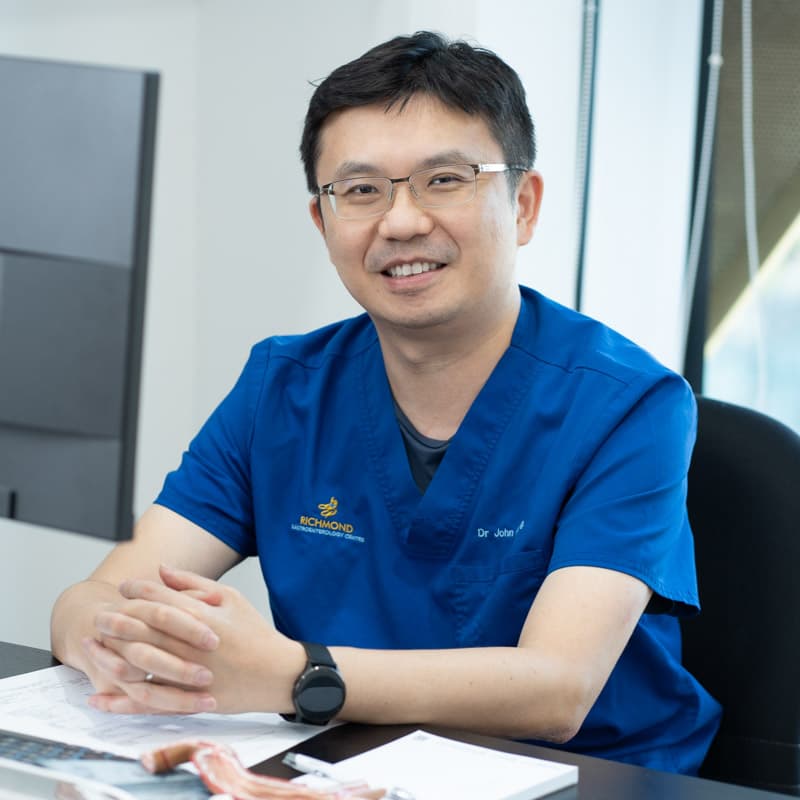
Dr. John Hsiang
MBChB (NZ), FRACP (Australasia), MD (Doctorate), FRCP (Edinburgh), FAMS (Gastro)
Dr. John Hsiang is a distinguished gastroenterologist in Singapore with extensive training and experience in digestive health. He obtained his Fellowship of the Royal Australasian College of Physicians in Gastroenterology in 2012 and holds a PhD in viral hepatitis and fatty liver disease research.
He provides care for a broad range of digestive and liver concerns, combining thorough evaluation with tailored management to support patients’ long-term well-being.
Dr Hsiang is skilled in performing gastroscopy (upper endoscopy) and colonoscopy to investigate symptoms, detect stomach and colon cancers at an early stage, and provide timely treatment options.
With a commitment to individualised care, he applies an evidence-based approach that prioritises accuracy, effectiveness and patient comfort at every stage of diagnosis and treatment.
Languages Spoken:
English, Mandarin and Hokkien
Fellowship Trained Specialist
20+ Years of Clinical Experience

What is a Gastroscopy?
Also known as an upper endoscopy, a gastroscopy allows the doctor to examine the oesophagus, stomach, and duodenum (the first part of the small intestine) using a thin, flexible tube with a camera.
It is essential for diagnosing a range of conditions, including Helicobacter pylori (H. pylori) infection, Gastroesophageal Reflux Disease (GERD) and early-stage digestive cancers, often before symptoms become severe.
Stomach and oesophageal cancers are among the most life-threatening when detected late, making early diagnosis through procedures such as gastroscopy key to improving treatment effectiveness and long-term outcomes.
How a Gastroscopy (Upper Endoscopy) is Performed
During the procedure, a thin, flexible tube called a gastroscope or endoscope is gently inserted through the mouth and guided down the throat. Attached to the endoscope is a camera that provides a clear, real-time view of the upper digestive lining.
This allows the specialist to inspect the tissues thoroughly and, if necessary, perform a biopsy to collect a small tissue sample for testing. Biopsies may be used to check for H. pylori infection, inflammation, precancerous changes or cancer.
If polyps or other abnormal growths are found, they can often be removed during the same procedure.
What to Expect Before, During and After a Gastroscopy
Before the Gastroscopy
- Our staff will assist with any required insurance pre-authorisations.
- Fasting for 6–8 hours is necessary to ensure your stomach is empty.
- Some medications may need to be paused or adjusted, as advised by your doctor.
- Arrange for someone to accompany you home, as sedation will be used during the procedure.
On the Day of the Gastroscopy
- The procedure is done under sedation for comfort.
- Patients are usually asleep during the procedure or comfortably sedated.
- A thin tube (endoscope) is guided through your mouth to examine the gastrointestinal tract.
- The specialist examines the lining and may take biopsies or remove polyps if necessary.
After the Gastroscopy
- You will be monitored in a recovery area until the sedation wears off.
- Mild throat discomfort or bloating may occur, but usually resolves within a few hours.
- Most patients can resume eating within a few hours after the procedure.
- Your doctor will review the findings and discuss results at a follow-up consultation.
How Safe is Gastroscopy?
Gastroscopy is a widely performed and generally safe procedure, especially when carried out by an experienced specialist. Gastroenterologists undergo extensive training to perform endoscopies with accuracy, care and a strong emphasis on patient safety.
Complications are rare, but like any medical procedure, potential risks exist. These may include:
- A mild sore throat or bloating
- Reactions to sedation
- Bleeding, especially if a biopsy is taken
- Perforation (a small tear in the digestive tract wall), which is very uncommon
Your safety is our priority. Patients are carefully assessed beforehand, and the procedure is performed using sterile, high-standard equipment. For most individuals, the benefits of accurate diagnosis and early detection far outweigh the minimal risks involved.
10-15 mins
Outpatient Procedure
Gastroscopy is a quick procedure that typically takes only 10 to 15 minutes to perform. In Singapore, it is commonly done as a day surgery under light sedation, allowing patients to return home the same day.
Within 7 Days*
Faster Access
Subsidised gastroscopy is available in public hospitals, but typically requires a referral and longer wait times. Private centres offer faster access, often within 7 days*.
* Some cases may require extra time for insurance pre-authorisation.
When is a Gastroscopy Necessary?
An upper endoscopy may be recommended for both diagnostic and surveillance purposes, depending on your symptoms and risk profile.
In Singapore, while there is no routine screening age for the general population, your doctor may recommend a gastroscopy if you experience persistent symptoms that do not resolve with initial treatment.
Your doctor may also recommend a gastroscopy if you experience:
- Persistent heartburn or acid reflux (GERD symptoms)
- Difficulty or pain when swallowing
- Upper abdominal pain or persistent bloating
- Persistent nausea or vomiting
- Unexplained weight loss or loss of appetite
- Signs of bleeding, such as vomiting blood or having black, tarry stools
- A family history of stomach cancer
Improving Outcomes Through Early Screening
Gastroscopy plays a vital role in the early detection and management of upper digestive conditions. In cases such as stomach or oesophageal cancer, early diagnosis can offer the possibility of a cure with timely treatment.
Similarly, identifying and treating conditions like GERD early can help prevent progression to more serious complications, such as Barrett’s oesophagus.
What to Expect: Your Gastroscopy Step-by-Step
Concerned about your digestive symptoms or gastrointestinal cancer risk? Book a screening to get evaluated by our gastroenterologist in Singapore.

Make an Appointment
Pre-Procedure Consultation
Undergoing the Gastroscopy
Post-Procedure Care and Follow-Up
Patient Information
Is a gastroscopy painful?
No, the procedure is not painful. It is performed with either a local anaesthetic throat spray or light sedation to ensure you are comfortable and most patients have little to no memory of it.
How long does a gastroscopy take?
The endoscopy itself is very quick, usually lasting only 10 to 15 minutes. However, you should plan to be at the clinic for a few hours to account for preparation and recovery from sedation.
What is the difference between a gastroscopy and a colonoscopy?
A gastroscopy (or upper endoscopy) examines the upper part of the digestive tract: the oesophagus, stomach and duodenum. A colonoscopy examines the lower part: the large intestine (colon and rectum).
Will I need someone to accompany me home?
Yes, if you receive sedation, you will need to arrange for someone to take you home. You will not be alert enough to drive or take public transport safely on your own.
Can I eat after the procedure?
You can typically resume a light diet a few hours after the gastroscopy, once the effects of the throat spray or sedation have worn off and you can swallow normally.
When will I get my results?
Your doctor will share the initial findings with you right after the procedure. If a biopsy was taken to test for H. Pylori or other conditions, the full lab results may take a few days to a week.
Can I go back to work the next day?
Yes, most patients can resume work and other normal activities the day after the procedure. It is advised to rest for the remainder of the day of the gastroscopy.
Consult Our Specialist
Experiencing digestive symptoms or discomfort? Speak to our gastroenterologist for a clearer understanding of your condition and treatment options.
You may book an appointment using our contact form or call the clinic at 6517 9958