When it comes to cancer, many people hope for a simple blood test that can confirm or rule out the disease. Tumour marker tests are often seen as that “shortcut”; while these tests prove to be valuable clues, they should not be used as standalone diagnostic tools.
Let’s unpark what tumour markers really tell you, when you should go for further scope testing, and when they can be helpful.
What are tumour markers?
Tumour markers are substances found in blood, urine, or tissue produced either by cancer cells themselves or by the body in response to cancer. Tumour marker tests are often used to help diagnose certain cancers, monitor the effectiveness of cancer treatment, or detect recurrence after treatment.
However, tumour markers alone are rarely conclusive and abnormal levels should prompt further testing, like scopes or imaging.
Common tumour markers and what they detect
| Tumour Marker | Limitations |
|---|---|
| AFP (Alpha-fetoprotein) Associated Cancer/s: Liver cancer, germ cell tumours (testicular/ovarian) |
Can also be elevated in liver diseases like hepatitis or cirrhosis. |
| CA-125 Associated Cancer/s: Ovarian cancer |
May also rise in endometriosis, pelvic infections, or menstruation. |
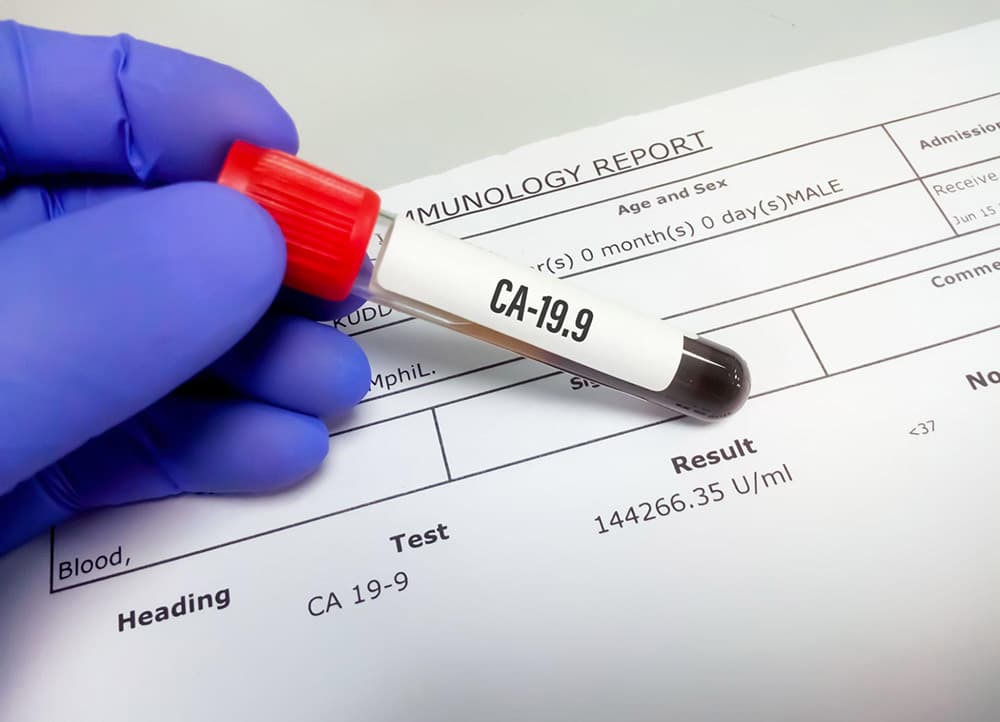
| CA 19-9 Associated Cancer/s: Pancreatic cancer, bile duct cancer, gastric cancer |
Can rise in non-cancerous conditions such as gallstones, pancreatitis. |
| CEA (Carcinoembryonic antigen) Associated Cancer/s: Colorectal cancer, lung, breast, and pancreatic cancer |
Also elevated in smokers and non-cancer conditions. |
| PSA (Prostate-specific antigen) Associated Cancer/s: Prostate cancer |
Can rise in benign prostate enlargement (BPH) or prostatitis. |
| hCG (Human chorionic gonadotropin) Associated Cancer/s: Testicular cancer, germ cell tumours |
Also elevated in pregnancy and some benign conditions. |
| Chromogranin A Associated Cancer/s: Neuroendocrine tumours |
Can rise with proton pump inhibitors. |
As you can see, each marker is linked to certain cancers. However, no single tumour marker test can detect all cancers, e.g. PSA is only useful for the prostate, CA-125 for ovarian cancer and not breast cancer.
How accurate are tumour marker tests?
Tumour marker tests are not 100% accurate. A high level doesn’t always mean cancer, and a normal level doesn’t always mean you’re cancer-free. Many tumour markers like CEA, CA 19-9 and CA 50 tend to rise only in the later stages of gastric cancer, which makes them less useful for early detection.
There is also the possibility of false positives (raised markers due to benign conditions like inflammation, infection, or stress) and false negatives (early-stage cancers may not produce enough markers to show up).
For the most accurate results, we often recommend confirmatory tests such as scopes, imaging scans or biopsies alongside tumour markers.
Should I do a scope instead of a tumour market test then?
While tumour marker tests are not meant to replace diagnostic procedures like scopes, imaging, or biopsies, they can serve as supportive tools:
- Tumour markers are not definitive. Elevated results may be due to non-cancerous conditions (e.g., inflammation, infection, or even lifestyle factors). A normal result also does not completely rule out cancer.
- Scopes provide direct visualisation. For example, a colonoscopy allows doctors to see and remove polyps before they become cancerous, while a gastroscopy checks for stomach or oesophageal issues that a blood test cannot detect.
Where a tumour marker test comes in helpful is when doctors need to monitor treatment response, check for recurrence, or guide further investigations when paired with symptoms or imaging results.
If you have persistent symptoms e.g. blood in stools, abdominal bloating, your doctor will likely recommend a scope or imaging regardless of your tumour marker levels.
In short, a tumour marker test can be a helpful screening tool, but a scope remains the primary and most reliable way for detecting and confirming cancer at an early and treatable stage.
Can stress cause tumour markers to rise?
Stress alone is unlikely to directly raise tumour markers. However, stress can affect your body in other ways, impacting immunity, hormones, and overall health. More commonly, tumour markers can be elevated due to non-cancerous conditions such as:
- Chronic inflammation
- Infections
- Liver disease
- Benign cysts or growths
Is the Lucence Multi-Cancer Detection Test more accurate than traditional tumour marker tests?
The Lucence Multi-Cancer Early Detection (MCED) test is a blood-based screening tool designed to detect multiple types of cancer from a single sample. Unlike traditional tumour marker tests that measure specific proteins associated with one or a few cancers, Lucence analyses circulating DNA fragments shed by cancer cells. This allows it to potentially identify a wider range of cancers, even at earlier stages.
While this approach can improve early detection and reduce the likelihood of false positives caused by benign conditions or inflammation, it is important to understand that Lucence is still a screening tool. It cannot confirm the presence, location, or stage of cancer.
For definitive diagnosis, scopes, imaging, and biopsies remain the primary diagnostic methods. Abnormal results from any blood-based test should always be followed up with these investigations to ensure accurate assessment and timely treatment.
Considering Getting Screened?
Tumour markers are valuable tools in cancer care—but they are not a substitute for diagnostic tests. They are most effective when combined with imaging, scopes, and professional medical guidance. If you’re considering screening, consult our gastroenterologist to explore the options that suit your age, risk profile, and current stage of life.
Many tumour markers like CEA, CA 19-9 and CA 50 tend to rise only in the later stages of gastric cancer, which makes them less useful for early detection. Tumour marker tests are not 100% accurate.
- Mazurek, A., Nikliński, J., Laudański, T., & Pluygers, E. (1998). Clinical tumour markers in ovarian cancer. European journal of cancer prevention : the official journal of the European Cancer Prevention Organisation (ECP), 7(1), 23–35.
- Roberts, P. J., Haglund, C., Onali, M., & Kuusela, P. (1989). Tumour markers in gastric cancer. Annales chirurgiae et gynaecologiae, 78(1), 38–40.