Barrett’s Oesophagus
Barrett’s oesophagus occurs when chronic acid reflux permanently changes the normal oesophageal lining into abnormal intestine-like cells.
Richmond Gastroenterology Centre
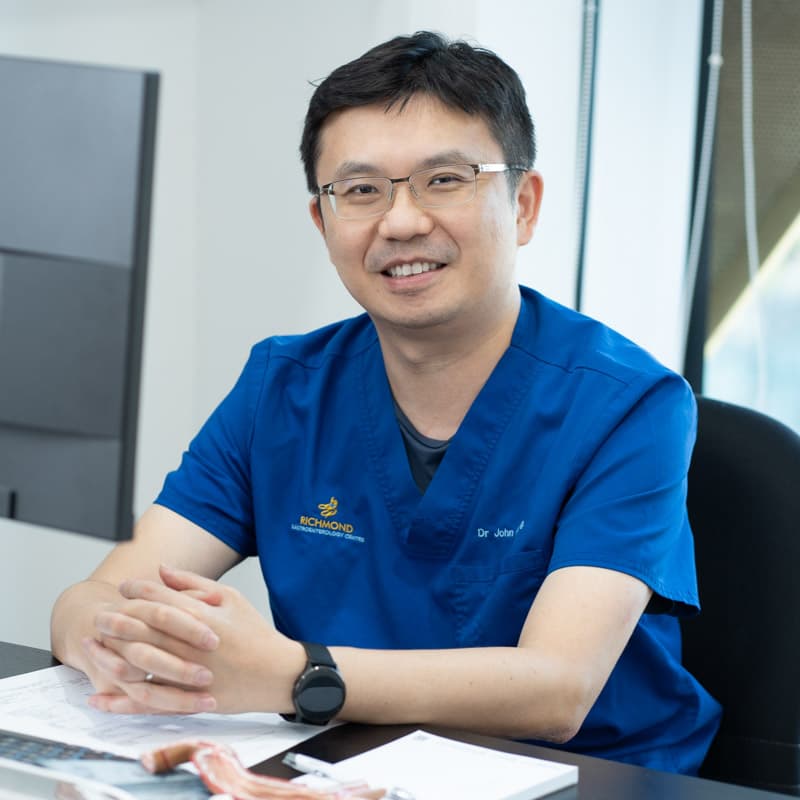
Dr. John Hsiang
MBChB (NZ), FRACP (Australasia), MD (Doctorate), FRCP (Edinburgh), FAMS (Gastro)
Clinical Expertise: Abdominal Pain & Bloating, Gastrointestinal Cancers, Gastroesophageal Reflux Disease, H. Pylori, Irritable Bowel Syndrome, Gallbladder Diseases
Dr. John Hsiang is a distinguished gastroenterologist, having obtained his Fellowship of the Royal Australasian College of Physicians in Gastroenterology in 2012. He holds a doctorate (PhD) in Viral Hepatitis and Fatty Liver Disease research.
Dr. Hsiang specialises in performing endoscopies and colonoscopies to investigate gastrointestinal symptoms, diagnose stomach and colon cancers, and deliver targeted treatment options.
Dr. Hsiang adheres to an evidence-based practice and a personalised approach, ensuring safe and optimal outcomes for his patients.
Languages Spoken:
English, Mandarin and Hokkien
Fellowship Trained Specialist
20+ Years of Clinical Experience

What is Barrett’s Oesophagus?
Barrett’s oesophagus is a condition where the normal lining of the oesophagus is replaced by abnormal intestine-like cells due to chronic acid reflux.
This change occurs when repeated exposure to stomach acid damages the oesophageal tissue, causing the body to replace it with cells that are more resistant to acid.
Whilst this adaptation initially protects against further damage, these abnormal cells have the potential to become cancerous over time.
The condition is diagnosed through endoscopy and confirmed by tissue samples showing intestinal metaplasia.
What Causes Barrett’s Oesophagus?
Barrett’s oesophagus develops as a result of chronic gastro-oesophageal reflux disease (GERD), where stomach acid repeatedly flows back into the oesophagus. Several factors increase the risk of developing this condition:
Primary risk factors include:
- Chronic GERD – long-term acid reflux is the main cause
- Age and gender – most common in men over 50
- Obesity – increases abdominal pressure and promotes acid reflux
- Smoking/Vaping – weakens the oesophageal sphincter and increases acid production
- Hiatal hernia – allows acid to escape more easily into the oesophagus
Symptoms and Diagnosis
Additional factors that may contribute include a family history of Barrett’s oesophagus or oesophageal cancer and certain dietary habits. The longer and more severe the acid reflux, the higher the risk of developing Barrett’s oesophagus.
Symptoms of Barrett’s Oesophagus
Barrett’s oesophagus itself typically causes no symptoms. However, it is often found in individuals with long-standing gastro-oesophageal reflux disease (GERD).
Common symptoms associated with underlying reflux include:
- Frequent heartburn or acid regurgitation
- Difficulty swallowing (dysphagia)
- Chest discomfort or a burning sensation behind the breastbone
- A sour taste in the mouth or bad breath
- Chronic cough or hoarseness, especially in the morning
Because Barrett’s oesophagus increases the risk of oesophageal cancer, regular monitoring is recommended for those diagnosed, especially if symptoms persist or worsen despite treatment.
How is Barrett’s Oesophagus Diagnosed?
Barrett’s oesophagus is diagnosed through an upper endoscopy (gastroscopy):
During this procedure, a thin, flexible tube with a camera is inserted through the mouth to examine the lining of the oesophagus.
If any areas appear abnormal, small tissue samples (biopsies) are taken for further analysis.
The diagnosis is confirmed when intestinal-type cells, which are not normally found in the oesophagus, are seen under the microscope.
This change is called intestinal metaplasia and is a key feature of Barrett’s oesophagus.
If Barrett’s oesophagus is confirmed, your doctor may recommend regular surveillance endoscopies to monitor for any signs of progression towards dysplasia or cancer.
How is Barrett’s Oesophagus Treated or Managed?
Management focuses on controlling acid reflux and monitoring for early signs of progression. Common approaches include:
- Long-term acid suppression using proton pump inhibitors (PPIs) to reduce reflux and inflammation.
- Lifestyle modifications such as weight management, avoiding trigger foods, eating smaller meals and not lying down after eating.
- Surveillance endoscopy at regular intervals to detect any changes in the oesophageal lining.
- Endoscopic treatment, such as radiofrequency ablation or endoscopic mucosal resection, may be recommended if precancerous changes (dysplasia) are found
Surgical options are rarely required but may be considered in selected cases with high-grade dysplasia or early cancer.
1-2%
Incidence Rate
Barrett’s oesophagus affects about 1% to 2% of the general population, and is more common in people with long-standing gastroesophageal reflux disease (GERD).
5-15%
Link to Chronic Reflux
Barrett’s oesophagus is diagnosed in approximately 5% to 15% of patients undergoing endoscopy for chronic reflux symptoms in Singapore, reflecting a similar trend seen in Western countries due to lifestyle and dietary shifts.
Prevention: When to See a Doctor
Barrett’s oesophagus is not reversible, so it is important to take precautionary steps if you are at risk. Managing chronic acid reflux early can help reduce the likelihood of changes to the oesophageal lining.
You should see a doctor if you experience persistent symptoms of gastro-oesophageal reflux, such as frequent heartburn, a sour taste in the mouth or chest discomfort after meals.
Difficulty swallowing, chronic throat irritation or a lingering cough may also warrant further evaluation.
If symptoms continue despite lifestyle changes or medication or if you are concerned about your long-term reflux history, speak to your doctor about whether an endoscopy is appropriate.
Early assessment supports timely intervention and long-term monitoring.
The Importance of Timely Medical Intervention
Barrett’s oesophagus primarily impacts men over 50 with long-standing GERD and increases oesophageal cancer risk by 30-40 times compared to the general population.
Early diagnosis and regular monitoring are essential to prevent cancer progression. An experienced gastroenterologist can accurately diagnose your condition, rule out other serious issues and develop a personalised management plan to help you find relief and prevent complications.
Our Treatment Process
Experiencing symptoms suggestive of Barrett’s Oesophagus? Here’s what to expect when you visit our gastroenterologist:

Make an Appointment
Specialist Consultation & Diagnosis
Your Personalised Treatment Plan
Ongoing Monitoring and Care
Patient Information
How often do I need surveillance endoscopy?
Without dysplasia: every 1-3 years. With low-grade dysplasia: every 6-12 months. High-grade dysplasia requires more frequent monitoring or immediate treatment.
Will I definitely develop oesophageal cancer?
No. Most people (over 95%) with Barrett's oesophagus never develop cancer. Regular monitoring helps detect changes early when treatment is most effective.
Can lifestyle changes help manage Barrett's oesophagus?
Yes. Weight loss, avoiding trigger foods, smaller meals, not lying down after eating and cutting out tobacco use can reduce reflux and slow progression.
Should I take acid-blocking medication indefinitely?
Most patients benefit from long-term PPI therapy to control reflux and potentially reduce cancer risk. Your doctor will determine the appropriate duration and dosage.
Is Barrett's oesophagus hereditary?
Not directly inherited, but a family history of Barrett's oesophagus or oesophageal cancer increases risk. Genetic factors may influence susceptibility to GERD development.
Can I still eat normally with Barrett's oesophagus?
Most people maintain a relatively normal diet, though you may need to avoid reflux triggers like spicy foods, citrus, chocolate, caffeine and alcohol.
What happens if dysplasia is found during surveillance?
Low-grade dysplasia requires more frequent monitoring. High-grade dysplasia typically needs endoscopic treatment to remove abnormal tissue and prevent cancer.
Are there any warning signs that Barrett's oesophagus is progressing?
New difficulty swallowing, unexplained weight loss, persistent chest pain, or changing reflux symptoms require immediate medical evaluation.
Can Barrett's oesophagus develop without reflux symptoms?
Yes, some people develop "silent reflux" without obvious heartburn symptoms, making regular screening important for those with risk factors.
Consult Our Specialist
Experiencing digestive symptoms or discomfort? Speak to our gastroenterologist for a clearer understanding of your condition and treatment options.
You may book an appointment using our contact form or call the clinic at 6517 9958