Oesophageal Cancer
Oesophageal cancer develops in the tube connecting the throat to the stomach and often progresses silently. It primarily affects men over 50 and is strongly linked to chronic acid reflux, smoking and heavy alcohol use.
Richmond Gastroenterology Centre
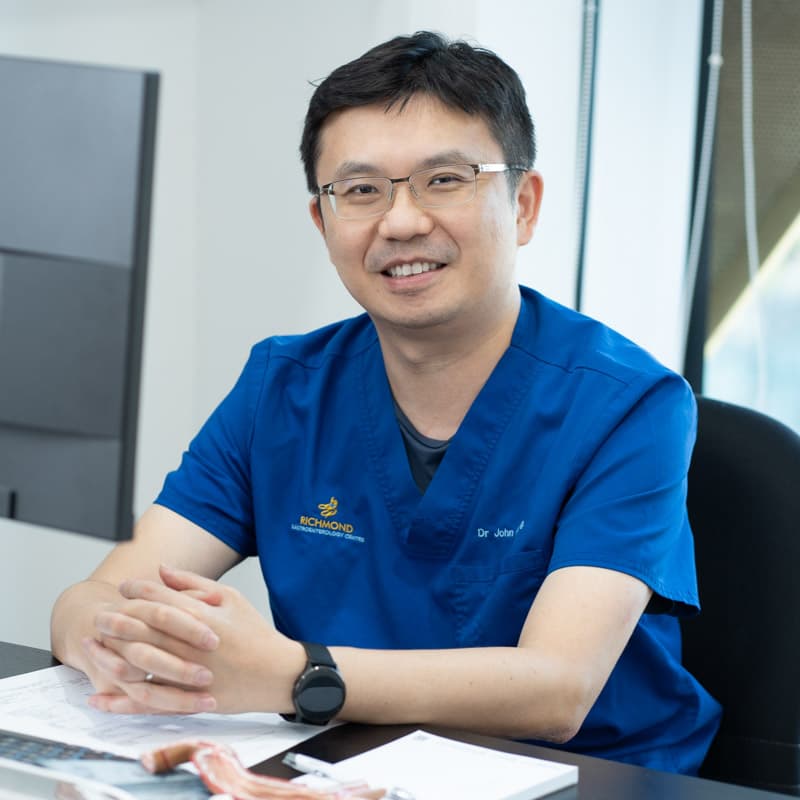
Dr. John Hsiang
MBChB (NZ), FRACP (Australasia), MD (Doctorate), FRCP (Edinburgh), FAMS (Gastro)
Dr. John Hsiang is a distinguished gastroenterologist in Singapore with extensive training and experience in digestive health. He obtained his Fellowship of the Royal Australasian College of Physicians in Gastroenterology in 2012 and holds a PhD in viral hepatitis and fatty liver disease research.
He provides care for a broad range of digestive and liver concerns, combining thorough evaluation with tailored management to support patients’ long-term well-being.
Dr Hsiang is skilled in performing gastroscopy (upper endoscopy) and colonoscopy to investigate symptoms, detect stomach and colon cancers at an early stage, and provide timely treatment options.
With a commitment to individualised care, he applies an evidence-based approach that prioritises accuracy, effectiveness and patient comfort at every stage of diagnosis and treatment.
Languages Spoken:
English, Mandarin and Hokkien
Fellowship Trained Specialist
20+ Years of Clinical Experience

Nasopharyngeal Cancer and Esophageal Cancer: What You Need to Know
While nasopharyngeal cancer (a type of head and neck cancer) and esophageal cancer are different diseases with different main causes, studies show that people who have had nasopharyngeal cancer have a 3 to 4 times higher risk of developing esophageal cancer later on. This increased risk is likely due to a combination of shared risk factors like smoking/vaping and alcohol use, genetic factors, and possibly even effects from cancer treatments.
Does Nasopharyngeal Cancer Change Esophageal Cancer Screening?
If you have chronic acid reflux (GERD) or reflux esophagitis, the presence of a past nasopharyngeal cancer diagnosis doesn’t change the standard recommendations for esophageal cancer screening. Typically, endoscopy for esophageal cancer isn’t routinely recommended for reflux unless you have Barrett’s esophagus or other high-risk features.
However, if you’re a survivor of nasopharyngeal cancer, especially if you also smoke or drink alcohol, it’s important for your doctor to be extra watchful for other cancers, including esophageal cancer. Your screening plan should always be tailored to your individual risk factors, including your cancer history and lifestyle choices.
Key takeaways:
- Nasopharyngeal cancer increases the risk of developing a second esophageal cancer.
- Shared risk factors like smoking and alcohol play a role.
- Existing guidelines for esophageal cancer screening in people with reflux don’t change.
- Survivors of nasopharyngeal cancer should be vigilant about overall cancer risk.
Remember to discuss your personal risk factors and screening options with your healthcare provider.
What Causes Oesophageal Cancer?
The exact cause of oesophageal cancer remains unclear, but it begins when cells in the oesophageal lining undergo mutations and grow uncontrollably. Major risk factors include chronic acid reflux (GERD), Barrett’s oesophagus, smoking, heavy alcohol use, obesity and poor diet.
Symptoms
Oesophageal cancer often develops silently in its early stages, with symptoms typically appearing only when the tumour has grown large enough to narrow the oesophagus.
The most common early symptom is difficulty swallowing (dysphagia).
Unintentional weight loss often accompanies swallowing difficulties, as patients may avoid eating due to discomfort.
Other significant symptoms include:
- Chest pain or discomfort – particularly when swallowing
- Persistent heartburn or acid reflux – that doesn’t respond to usual treatments
- Chronic cough or hoarseness
- Regurgitation of food
- Fatigue and weakness
How is Oesophageal Cancer Diagnosed?
Diagnosing oesophageal cancer typically involves several tests to confirm the presence of cancer, determine its type, and assess how far it has spread.
The primary diagnostic procedure is an endoscopy, where a thin, flexible tube with a camera examines the oesophagus directly.
Tissue samples (biopsies) are taken from suspicious areas for laboratory analysis.
Additional diagnostic tests include:
- Barium swallow – X-ray imaging after drinking a contrast solution
- CT scan – detailed images to assess tumour size and spread
- PET scan – identifies cancer cells throughout the body
- Endoscopic ultrasound – determines how deeply the cancer has penetrated
- Blood tests – assess overall health and organ function
Staging follows diagnosis to determine the cancer’s extent from Stage 0 (very early) to Stage IV (advanced), which is crucial for planning the most appropriate treatment approach.
When to See a Doctor
Early detection greatly improves outcomes in oesophageal cancer. Consult your doctor promptly if you experience:
- Persistent symptoms lasting over 2–3 weeks, especially swallowing difficulties that do not improve
- Worsening dysphagia—progressing from difficulty with solids to liquids
- Severe or increasing chest discomfort, particularly when eating or swallowing
- Unexplained weight loss, especially when accompanied by other symptoms
- Chronic acid reflux that does not respond to standard treatment
Seek urgent medical care if you:
- Are unable to swallow liquids or saliva
- Experience severe chest pain
- Have difficulty breathing
If you have multiple risk factors, such as long-standing GERD or a family history of oesophageal cancer, consider discussing screening options with your doctor, even if you do not have symptoms.
Early evaluation enables timely diagnosis and may reduce the need for more intensive treatment.
7th and 13th
Incidence Rate
Oesophageal Cancer Treatment
Treatment for oesophageal cancer depends on the cancer’s stage, location, type and the patient’s overall health. A multidisciplinary team of oncologists, surgeons and digestive care specialists develops the most appropriate treatment plan for each individual.
Surgery is often the primary treatment for early-stage cancers, with oesophagectomy (removal of part or all of the oesophagus) being the main approach, sometimes combined with reconstruction of the digestive pathway.
Main treatment options include:
- Chemotherapy – uses drugs to destroy cancer cells
- Radiotherapy – high-energy beams target cancer cells
- Chemoradiotherapy – a combination treatment, sometimes used instead of surgery
- Targeted therapy – drugs targeting specific cancer cell characteristics
- Immunotherapy – helps the immune system fight cancer
For advanced cases, treatment focuses on palliative care to manage symptoms and improve quality of life, including procedures to help with swallowing, such as stent placement.
The treatment team provides comprehensive supportive care, including nutritional support, pain management and psychological support throughout the treatment journey.
The Importance of Timely Medical Intervention
Oesophageal cancer develops in the tube connecting the throat to the stomach and often progresses silently. It primarily affects men over 50 and is strongly linked to chronic acid reflux, smoking and heavy alcohol use.
Early detection is crucial, as survival rates drop dramatically from over 40% when caught early to less than 5% in advanced stages.
What to Expect During Treatment

Make an Appointment
Comprehensive Testing and Diagnosis
Personalised Treatment Development
Ongoing Care and Support
Patient Information
What is the survival rate for oesophageal cancer?
Survival depends on the stage at diagnosis. Early-stage oesophageal cancer has a five-year survival rate of over 40%, while advanced-stage disease has a rate of less than 5%. Overall, the average five-year survival is around 20%.
Can oesophageal cancer be prevented?
Is oesophageal cancer hereditary?
Most cases aren't hereditary, though certain genetic conditions and family history can slightly increase risk. Most cases occur without a family history.
How quickly does oesophageal cancer spread?
Oesophageal cancer can be aggressive and spread relatively quickly to nearby lymph nodes and organs. Early detection is crucial.
What is Barrett's oesophagus and how does it relate to cancer?
Barrett's oesophagus is a precancerous condition caused by chronic acid reflux. It increases adenocarcinoma risk and requires regular monitoring.
Can you live normally after oesophageal cancer treatment?
What are the side effects of oesophageal cancer treatment?
Side effects may include difficulty swallowing, eating changes, fatigue, nausea and voice changes. Your medical team helps manage these effects.
How is oesophageal cancer different from throat cancer?
Consult Our Specialist
Experiencing digestive symptoms or discomfort? Speak to our gastroenterologist for a clearer understanding of your condition and treatment options.
You may book an appointment using our contact form or call the clinic at 6517 9958