Pancreatitis
Pancreatitis can transform everyday activities into painful ordeals, leaving you doubled over in agony and fearful of your next meal. This serious inflammatory condition of the pancreas affects thousands of Singaporeans each year, yet many suffer in silence, unaware that effective treatment options exist.
Richmond Gastroenterology Centre
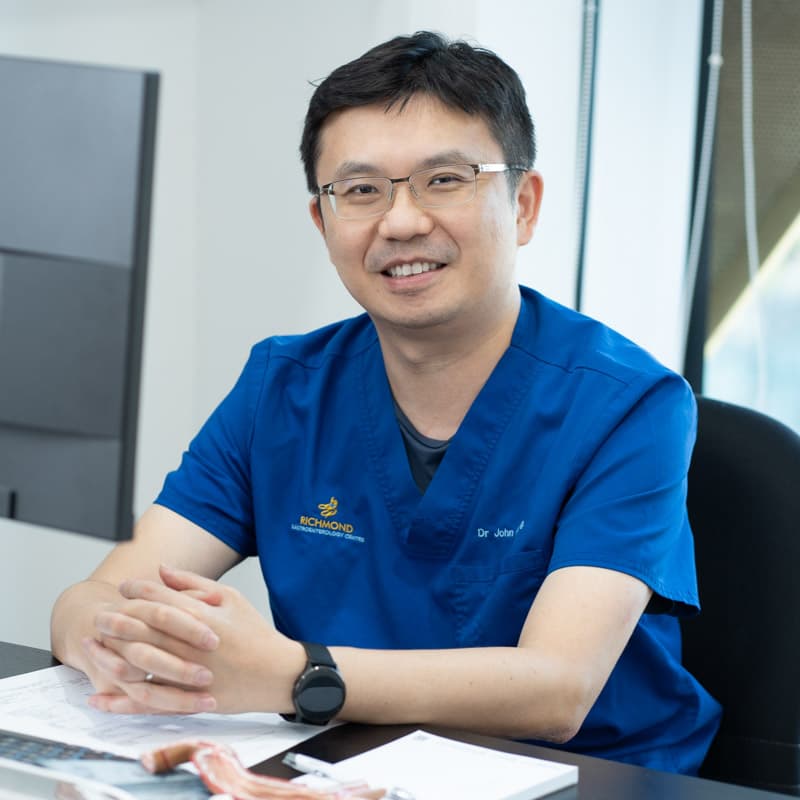
Dr. John Hsiang
MBChB (NZ), FRACP (Australasia), MD (Doctorate), FRCP (Edinburgh), FAMS (Gastro)
Dr. John Hsiang is a distinguished gastroenterologist in Singapore with extensive training and experience in digestive health. He obtained his Fellowship of the Royal Australasian College of Physicians in Gastroenterology in 2012 and holds a PhD in viral hepatitis and fatty liver disease research.
He provides care for a broad range of digestive and liver concerns, combining thorough evaluation with tailored management to support patients’ long-term well-being.
Dr Hsiang is skilled in performing gastroscopy (upper endoscopy) and colonoscopy to investigate symptoms, detect stomach and colon cancers at an early stage, and provide timely treatment options.
With a commitment to individualised care, he applies an evidence-based approach that prioritises accuracy, effectiveness and patient comfort at every stage of diagnosis and treatment.
Languages Spoken:
English, Mandarin and Hokkien
Fellowship Trained Specialist
20+ Years of Clinical Experience

Don’t Let Pancreatitis Control Your Life
Severe abdominal pain that radiates to your back, persistent nausea and unexplained weight loss may indicate pancreatitis – a serious inflammatory condition affecting the pancreas. While many dismiss these symptoms as routine digestive upset, untreated pancreatitis can lead to diabetes and other life-threatening complications.
Early diagnosis and proper treatment are essential for preventing long-term consequences and restoring your quality of life.
What is Pancreatitis?
Pancreatitis occurs when your pancreas becomes inflamed, essentially causing this organ to attack itself. The pancreas produces digestive enzymes that normally break down food in your small intestine; however, when inflammation strikes, these enzymes activate prematurely and begin digesting pancreatic tissue instead.
Your pancreas serves dual roles: producing enzymes for breaking down fats, proteins and carbohydrates and manufacturing hormones like insulin to regulate blood sugar. Acute pancreatitis strikes suddenly with intense symptoms but often resolves with proper treatment, while chronic pancreatitis develops gradually, causing permanent damage. Sudden onset of severe symptoms is commonly called a pancreatitis “attack” – requiring immediate medical attention. In Singapore, gallstones and alcohol consumption remain the primary causes.
Recognising the Warning Signs
Pancreatitis symptoms vary significantly depending on whether you’re experiencing acute or chronic inflammation, and recognizing these differences is crucial for seeking appropriate care.
Acute Pancreatitis Symptoms
Acute pancreatitis typically announces itself with severe upper abdominal pain that radiates straight through to your back. This isn’t ordinary stomach discomfort; patients often describe it as the worst pain they’ve ever experienced. The pain intensifies after eating, particularly fatty meals, and doesn’t improve with typical remedies like antacids or position changes.
Accompanying symptoms include:
- Persistent nausea and vomiting that provides no relief
- Fever and rapid pulse
- Extreme abdominal tenderness
- Being doubled over, unable to find any comfortable position
Chronic Pancreatitis Symptoms
Chronic pancreatitis presents more subtly with ongoing abdominal pain that waxes and wanes over time. Common signs include:
- Unexplained weight loss despite maintaining normal eating habits
- Oily stools that float and smell particularly foul
- New-onset diabetes as your pancreas loses its ability to produce insulin effectively
Some patients develop what gastroenterologists call pancreatic diabetes – a specific form of diabetes resulting from pancreatic damage rather than insulin resistance. This condition requires specialized management different from typical Type 1 or Type 2 diabetes.
Risk Factors
Several factors can trigger pancreatic inflammation, and recognising these triggers helps determine both treatment approach and prevention strategies.
Gallstones represent the leading cause of acute pancreatitis in Singapore. These deposits can block the pancreatic duct, causing enzymes to accumulate and inflame surrounding tissue.
Alcohol consumption ranks as the second most common cause, responsible for both acute episodes and chronic pancreatitis development. Even moderate drinking can trigger attacks in susceptible individuals.
High triglyceride levels can overwhelm the pancreas when blood fat levels exceed 500 mg/dL. This condition is becoming more prevalent in Singapore as diabetes and metabolic syndrome rates continue climbing. Certain medications, including some antibiotics, blood pressure drugs and immunosuppressants, occasionally trigger pancreatitis as an unexpected side effect.
Diagnosing Pancreatitis
At Richmond Gastroenterology Centre, we employ a comprehensive approach to diagnose pancreatitis and develop the most effective treatment plan for each patient.
Our evaluation begins with a detailed consultation examining your symptom pattern, medical history, family background and lifestyle factors. This comprehensive review helps us understand potential triggers and assess your individual risk profile for developing complications.
Laboratory testing forms a cornerstone of our diagnostic approach. We measure specific pancreatic enzymes like lipase and amylase, which become elevated during acute inflammation. Additional blood work screens for diabetes, nutritional deficiencies and other complications that might influence your treatment plan.
Advanced imaging studies provide detailed visualisation of your pancreas and surrounding structures. CT scans offer excellent detail for assessing inflammation and complications, while MRI provides superior soft tissue contrast for evaluating chronic changes. When indicated, endoscopic ultrasound allows us to examine pancreatic ducts and tissue with exceptional precision.
For complex cases requiring therapeutic intervention, we may recommend ERCP (Endoscopic Retrograde Cholangiopancreatography) to directly examine pancreatic ducts and perform treatments like gallstone removal or pseudocyst drainage.
20-30
The incidence of acute pancreatitis is estimated at 20–30 cases per 100,000 people per year, which likely translates to around 1000–1500 new cases annually in Singapore.
10-15%
Treating and Managing Pancreatitis
The treatment for pancreatitis varies based on whether you’re experiencing acute or chronic disease, the underlying cause and your individual health.
Here’s what you can expect during your consultations with our liver and pancreas specialist in Singapore:
Acute Pancreatitis Management
Immediate stabilisation often requires hospitalisation for comprehensive pain control, intravenous fluid resuscitation and careful nutritional management. We monitor your condition closely to detect complications early and adjust treatment accordingly.
Addressing underlying causes represents a critical component of acute care:
- Removing gallstones through endoscopic procedures
- Discontinuing trigger medications
- Treating conditions like high triglycerides that precipitated your episode
Nutritional rehabilitation requires careful reintroduction of feeding once inflammation begins subsiding. We work closely with dietitians to ensure proper nutrition while allowing your pancreas adequate recovery time.
Chronic Pancreatitis Care
Pain management for chronic pancreatitis demands a multifaceted approach:
- Medications for pain control
- Dietary modifications
- Sometimes minimally invasive procedures to interrupt pain pathways
Our goal is achieving sustainable pain control while maintaining your ability to function normally.
Enzyme replacement therapy becomes essential when your pancreas can no longer produce adequate digestive enzymes. These supplements, taken with every meal, dramatically improve digestion and prevent the malnutrition that would otherwise develop.
Diabetes management requires specialised expertise when it results from pancreatic damage rather than typical insulin resistance. We coordinate closely with endocrinologists to optimise blood sugar control while managing the unique challenges of pancreatic diabetes.
The Importance of Timely Medical Intervention
Delaying treatment for pancreatitis can lead to severe complications that may become life-threatening. Acute pancreatitis can progress to pancreatic necrosis, where portions of the pancreas die, potentially requiring surgical intervention. Chronic pancreatitis gradually destroys the pancreas’s ability to produce digestive enzymes and insulin, leading to malnutrition and diabetes.
Early medical attention can prevent these complications and significantly improve your long-term prognosis. Modern treatment approaches focus on managing symptoms, addressing underlying causes, and preventing recurrence through lifestyle modifications and appropriate medical therapy.
What to Expect During Treatment

Make an Appointment
Comprehensive Testing and Diagnosis
Personalised Treatment Development
Ongoing Care and Support
Patient Information
How can I tell if my stomach pain is actually pancreatitis?
Will my pancreatitis require surgery?
Can I ever drink alcohol again after pancreatitis?
How long does pancreatitis recovery take?
Acute pancreatitis recovery typically spans several days to weeks with appropriate treatment. Chronic pancreatitis requires ongoing management but many patients achieve excellent symptom control and maintain active, fulfilling lives.
Will I develop diabetes from my pancreatitis?
What dietary changes do I need to make?
Is pancreatitis hereditary in families?
How often will I need follow-up appointments?
Will insurance cover my pancreatitis treatment?
What should I do if my symptoms suddenly worsen?
Consult Our Specialist
Experiencing digestive symptoms or discomfort? Speak to our gastroenterologist for a clearer understanding of your condition and treatment options.
You may book an appointment using our contact form or call the clinic at 6517 9958